So you’re doubtlessly wondering why the following column appears now, apparently so dismissive of 2019, which is the newest year we’re all worrying about.
One reason harkens back to my early journalistic years at a community newspaper, where we were forbidden to use the phrase “ ‘Tis the season” in a headline more than once a year. Hence, we copy editors would race to deploy it as quickly as possible, usually the day after Thanksgiving. One year, I managed to sneak in “ ‘Tis the season: It’s Santa’s time to reign, dear,” thus managing to use both the coveted phrase and a nasty pun at one fell swoop.
Thus, this is a thinly veiled attempt to get the jump on what is likely to be a slew of columns, articles and prognostications on what the next decade will look like for HIT.
And, on a more serious note, it is important to think about what will be expected deliverables for HIT in the new decade. Expectations will be high from administrators, clinicians and consumers; and the healthcare industry will be under pressure to do things with technology that achieve startling progress in cutting costs, improving care and boosting efficiency. In short, there will be serious demands on HIT—technology will be expected to deliver after years of investment, patience and technological advancements. Thus, 2019 will be a year for HIT executives to sharpen their focus on what will be required of their IT systems in the 10 years beyond.
This is not an exhaustive list, but it’s clear that the 2020s will be a time for IT to pay up in healthcare.
Technology makes clinicians’ lives easier. A survey from the AMA this year continues to show that clinical systems are one of the chief reasons for physician burnout. This cannot continue—IT will need to prove it can reduce workloads for doctors and nurses, through easier interfaces, automated transcription, facilitated documentation and superior user experience.
Interoperability on steroids. The current push to achieve interoperability often ends the discussion at facilitating the movement of some patient data from point A to point B. For interoperability to truly pay off, patient information must be accessible and actionable for any relevant clinician, inserted into workflow and seamlessly moving from one records system to another, semantically meaning the same thing so there are no errors in communication. There are multiple technical hurdles here, ranging from employing technology (perhaps blockchain) to resolving patient identification issues.
Enabling patients as consumers. By the mid-2020s, the nation’s consumers will have had more than 15 years of experience using technology to make purchases, book flights, interact with companies and support their lives. They will have no patience for a healthcare system that can’t answer simple questions, like exactly how much a procedure will cost or why a consult with a clinician can’t be virtual. As consumers take on more of the burden of paying for their care, these incapabilities won’t be tolerated. Care will need to be seamless—available either at the wrist through a smart watch, in the hand with a smart phone, or in the home with remote equipment seamlessly interfaced with other clinical systems.
AI integral to healthcare. Artificial intelligence is showing promise in isolated tests in use cases. Until it’s validated, some clinicians fear that it could usurp their ability to treat patients. In the 2020s, AI and other advanced technologies will need to be deployed to augment clinicians’ abilities to spot medical issues, find the best treatments, and proactively care for patients. Platforms will need to be developed that enable algorithms to be massively used against patient data to post reliable warning flags, becoming smarter all the while.
Enabling smarter clinical trials. The clinical trial process to match patients with new treatments and drugs is still mired in an expensive trial-and-error world. In the new decade, this process needs to be efficiently automated, speeding clinical discovery and validation, and then enabling clinicians to link these emerging treatments to patients.
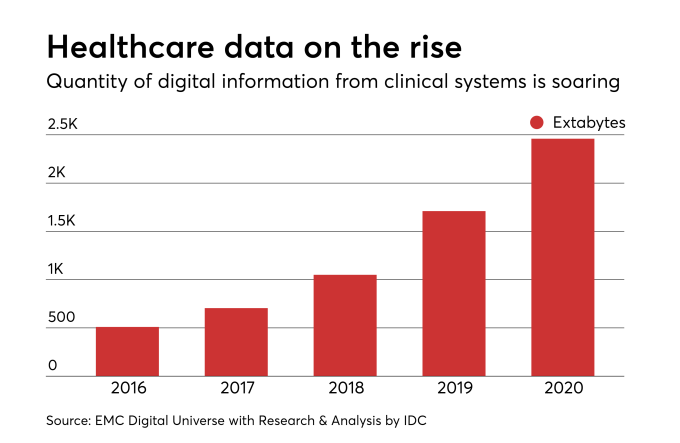
Factoring in new patient data. There will be an exponential increase in the data available on patients, ranging from that obtained from whole genome sequencing (which will become less expensive and more common) to data that now is difficult to include in systems, such as social determinants of health and patient-generated data. All this information will be crucial in getting a full picture of the patient for treatment.
EHR reinvention. Let’s face it; the current systems in place were designed to capture information intended to assist charge capture and billing. Current systems will need to morph—or be completely reinvented—to contain, and do something with, the massively growing data files that will represent each patient.
Extensive use of predictive analytics. Organizations’ IT systems will need to be able to look ahead with analytics and intervene in patient care before indications arise. This will mean using data to stop crisis events, such as sepsis and cardiac arrests, but also looking out months, perhaps years, into the future to engage patients actively in their own preventive care.
Supporting population health/value-based care. These initiatives will merge and become more serious in the future, as vestiges of fee for service go the way of the dinosaur. Provider organizations will need to completely master the ability to optimize care to multiple specific populations, and they’ll need souped-up IT systems to support them.
Quality will be king. As consumers become wiser shoppers for healthcare, they’ll look for quantifiable proof that healthcare providers are of the highest quality. Providers will need to be able to demonstrate quality with data, without excuses.
Of course, there will be more. Our limited minds can’t see everything that’s possible with IT in the next 10 (well, 11) years. ‘Tis the season to plan boldly and wildly, so ancient copy editors say.

