Naresh Tinani loves his job as a perfusionist at a hospital in Saskatchewan’s capital. To him, monitoring patient blood levels, heart beat and body temperature during cardiac surgeries and intensive care is a “privilege” — “the ultimate interaction between human physiology and the mechanics of engineering.”
But Tinani has also been on the other side of the system, like when his now-15-year-old twin daughters were born 10 weeks early and battled infection on life support, or as his 78-year-old mother waits months for new knees amid the coronavirus pandemic. While stressful, those moments helped make him “very proud” of his nation’s health care system, a cornerstone of Canadian national identity. He’s proud because during times of true emergency, he said the system took care of his family without adding cost and affordability to his list of worries.
And on that point, few Americans can say the same.
Before the coronavirus pandemic hit the U.S. full speed, fewer than half of Americans — 42 percent — considered their health care system to be above average, according to a PBS NewsHour/Marist poll conducted in late July. Roughly as many people — 49 percent — said the Canadian system was better than their own. Compared to people in most developed nations, including Canada, Americans have for years paid far more for health care while staying sicker and dying sooner.
In the United States, unlike most countries in the developed world, health insurance is often tied to whether or not you have a job. More than 160 million Americans relied on their employers for health insurance before COVID-19, while another 30 million Americans were without health insurance before the pandemic.
Tens of millions more Americans lost their health care coverage when coronavirus fears triggered a recession this year. Numbers are still shaking out, but one projection from the Urban Institute and the Robert Wood Johnson Foundation suggested as many as 25 million more Americans became uninsured in recent months. That study suggested that millions of Americans will fall through the cracks and may fail to enroll for Medicaid, the nation’s safety net health care program, which covered 75 million people before the pandemic.

How do health care prices in the United States compare to those in other countries? The price tag for common procedures can be staggeringly different, depending on where the patient receives care. Test how much you know with this quiz.
When people debate how to fix the broken U.S. system (an especially common conversation during presidential election years), Canada invariably comes up — both as an example the U.S. should admire and as one it should avoid. During the 2020 Democratic primary season, Sen. Bernie Sanders touted Canada’s single-payer model as the antidote needed to heal the U.S. health care system, pitching his own version called “Medicare for All.” Sanders dropping out of the race in April fueled speculation that Biden might adopt a more progressive platform, including on health care, to woo Sanders’ diehard supporters.
Every health care system has its strengths and weaknesses, including Canada’s. Here’s how that nation’s system works, why it’s admired (and sometimes disparaged) by some in the U.S., and why outcomes in the two countries have been so different during the COVID-19 pandemic.
How Canada developed its system
The Canadian health system hasn’t always been this way; it was born out of need in a time of economic crisis. In 1944, voters in the rural province of Saskatchewan, hard-hit during the Great Depression, elected a democratic socialist government after politicians had campaigned for a basic right to health care. At the time, people felt “that the system just wasn’t working” and they were willing to try something different, said Greg Marchildon, a health care historian who teaches health policy and systems at the University of Toronto.
Three years later, the same politicians, led by Saskatchewan Premier Tommy Douglas, replaced the privately insured and funded health care system and instead used taxes to cover all hospital care province-wide. The change was met with pushback. On July 1, 1962, doctors staged a 23-day strike in the provincial capital of Regina to protest universal health coverage. But ultimately, the program “had become popular enough that it would become too politically damaging to take it away,” Marchildon said.
Other provinces took notice. Those efforts spread nationwide and eventually established what would become the Canadian health care system, known as Medicare, through the Canada Health Act of 1984.
Under this law, Canada’s 13 provinces and territories control their health care, meaning those governments get to decide how to design and deliver their health care system — not unlike Medicaid in the U.S, which is managed by the states. To receive federal dollars, provinces and territories must meet five basic criteria: public administration, comprehensiveness, universality, portability and accessibility. If you move between provinces — from Toronto to Vancouver, for instance — your insurance travels with you. Everyone (except undocumented immigrants) carries a health insurance card that covers them. These plans cover medically necessary hospital care and essential physician services, but do not include dental, out-of-hospital medications, long-term care, ambulance services or vision care — a big sticking point in the current Canadian debate over health care. To pay for uncovered care, two-thirds of Canadians rely on supplemental insurance plans typically paid by employers (as is the case in much of the U.S.).
Who has coverage?
Today, severe job losses do not leave people completely uninsured in Canada, said Colleen Flood, who directs the University of Ottawa’s Centre for Health Law, Policy and Ethics. Amid the pandemic, Canadians can get tested for the virus when they need it and they don’t fear that the cost of a test or treatment could financially break them if COVID-19 doesn’t kill them first, Flood said: “Coast to coast, every Canadian has the security of health care for them if they do get sick.”
“To Canadians, the notion that access to health care should be based on need, not ability to pay, is a defining national value,” Dr. Danielle Martin, chief medical officer at Women’s College Hospital and professor at the University of Toronto, wrote in a 2018 Lancet article that unpacked the Canadian health care system.
Americans simply don’t live with that confidence, Flood said. Losing a job is “bad enough, but to imagine that you’re going to have to lose everything you’ve got to qualify for Medicaid. Sell your house. Sell your car and basically be on the bones of your ass before you get any medical coverage.”
“It’s a human right to have access to health care,” Flood said.
Cheryl Camillo, a former technical director for the Centers for Medicare and Medicaid Services, came from Maryland to the University of Regina in Saskatchewan to learn about the roots of the Canadian health care system and how the U.S. and Canadian systems can benefit from each other. Camillo said Americans could benefit from the Canadian system with “less paperwork, less red tape, less cost for sure, even after factoring in taxes, more convenience, more choice, more opportunity in work lives, more time and more happiness and more social cohesion and more value.”
Most Canadians understand their system requires tradeoffs, including wait times of months for certain procedures or treatment, Martin told the NewsHour. For instance, to protect its universal access, Canadian law forbids people from buying additional insurance to cover hospital care.
It is a law that Vancouver-based orthopedic surgeon Dr. Brian Day has fought in court since 2009. He has set up private hospitals in Canada and in the U.S. to offer elective surgeries and to reduce waitlists filled with the hundreds of people wanting procedures. Day, who argues for more private dollars in his nation’s health care system, said that the Canadian system doesn’t offer enough coverage, noting that people still have to seek private insurance for services not covered by the Canada Health Act, such as dentistry, mental health care or medications not prescribed in a hospital (though they do cost less than in the U.S.). He says people are dying while waiting for treatment, pointing to data from the Canadian Institute for Health and Information that suggested Canadian patients wait for some procedures four times longer than those in France, and thinks that those who are willing to pay should be able to get services sooner. Even in Canada, “The biggest determinants of health is wealth,” he added. And yet, Day doesn’t see what is happening south of his border as a better approach.
“Neither the Canadian or the U.S. are the models that should be looked at,” he said. Where we should be looking: Switzerland, he said. The country allows private health insurance, but if a person is unable to pay, the government pays their premiums for them, Day said, out of tax money and other funds. “The thing that is wrong with the U.S. is it needs universal health care.”
Cost
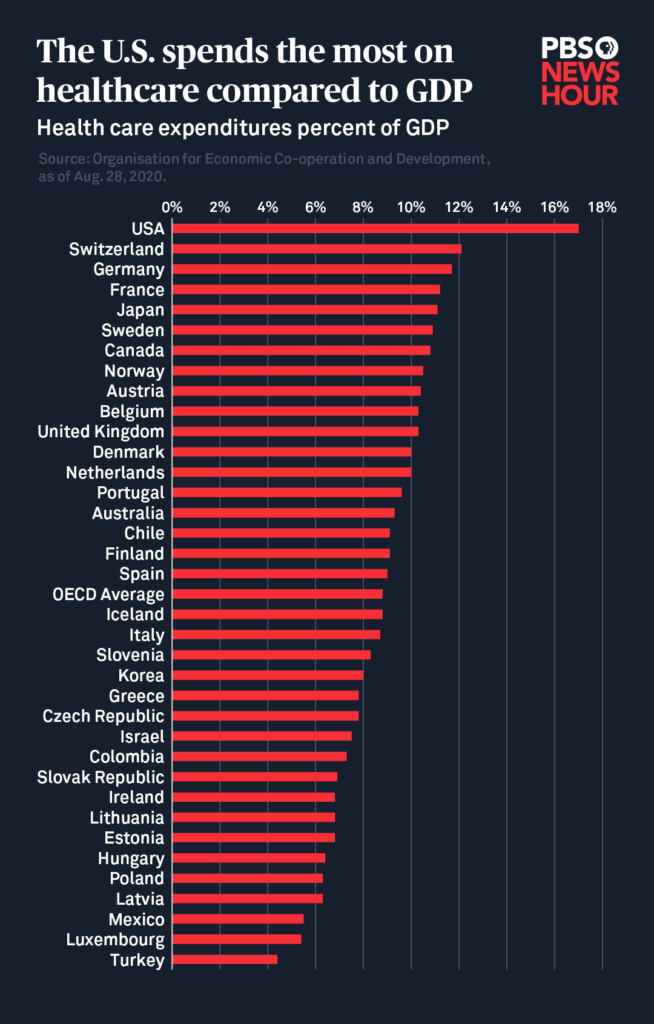
In 2019, health expenses drove more Americans into bankruptcy than any other reason, according to the American Journal of Public Health. That same year, health care consumed 17 percent of the U.S. gross domestic product, a greater share than in any other developed country, including Canada, which was at 10.8 percent, according to the latest OECD data.
Canadians don’t typically worry about medical bankruptcy. If you get hit by a bus and receive any form of hospital care, you’re billed nothing. Taxes cover the cost of hospital care, such as emergency room visits or operations to remove tumors.
Patient advocate Carolyn Canfield, who lives in British Columbia, has had to confront a life-threatening cancer diagnosis, but not the endless medical costs that many in the U.S. face. Born and raised in the U.S., after Canfield emigrated to Canada after college. More than a decade ago, she noticed suspicious symptoms. She saw her doctor who referred her for testing. The biopsy revealed a malignant growth, and her doctor referred her to a specialist.
“That cost me $ 0. I had no out-of-pocket expenses,” she said. “I never saw a bill.”
Wait times
In early March, Naresh Tinani’s 87-year-old mother had been waiting four months to replace her knee cap. Age and osteoporosis had taken their toll, and she was ready for the relief an elective surgery would bring, he said. She underwent diagnostic tests and consulted with doctors. Within three days of her operation, Tinani said, Canada entered lockdown due to COVID-19 and hospitals stopped conducting elective surgeries. Several more months passed. After the country began easing lockdown restrictions, the hospital contacted Tinani’s mother to see if she wanted to go forward with her surgery. However, because of her age, concerns about the virus and coordinating family members to care for her during her recovery, Tinani said his mother chose to postpone her knee replacement. It’s now been nearly a year since she first sought out the procedure, and she’s not sure when the surgery will be possible again.

Left to right: Robin Tinani stands over her newborn daughter, Mira, in the NICU. Mira and her twin sister, Jaya, were born 10 weeks premature and fought infections after birth. They received weeks of care in the Canadian hospital system, and their family was charged nothing. Naresh Tinani, a perfusionist at Regina Qu’Appelle Health Region in Saskatchewan, attends a sporting event with his mother, Nirmala Tinani. His mother, 87, has waited for roughly a year to undergo knee replacement surgery, an elective procedure. Photos courtesy of Naresh Tinani
The amount of time Canadians wait for medical care depends on the type of procedure, and wait times have shifted over time. The Canadian Institute for Health Information tracks provincial-level data on wait times for elective procedures for non urgent outpatient specialty services, such as cataracts and hip replacements. Some provinces are better at meeting benchmarks than others. However, “Canadians are not dropping dead” as a result, Martin said.
At the same time, a senior with bad or painful arthritis may have to wait a year for hip replacement surgery, Martin said.
“It’s a real problem in Canada and not one we should sugar-coat,” she said.
For roughly 20 years, Wendell Potter worked to sow fear of the Canadian health care system — including long wait times like these — in the minds of Americans. As the head of corporate communications for health insurance giant Cigna, Potter said industry executives felt the public Canadian system exposed shortcomings in the private U.S. health system and potentially threatened their profits.
That led Potter and his peers to perpetuate the idea that wait times forced Canadians to forgo needed medical care and live in peril. Potter said he and his colleagues cherry-picked data and obscured the bigger picture, but to get that mischaracterization to take root in people’s imagination, “there needs to be a kernel of truth there,” he said.
In this case, Canadians at the time experienced longer wait times for non-emergency elective procedures, such as knee and hip replacements. Massive health insurance companies poured money into promoting this idea until it bloomed into a mischaracterization of the entire Canadian health care system.
The trick to getting misinformation to stick is to “repeat it over and over and over again, over years, and get friends to repeat it,” Potter said.
Eventually, Potter’s conscience got the better of him, he said. In 2008, he abandoned corporate communications after he was told to defend a company decision not to pay for the liver transplant of 17-year-old Nataline Sarkisyan, despite doctors saying the procedure would save her life. She died. He is now president of Medicare for All Now, an advocacy group that promotes universal health coverage.
“We wanted people to think they needed to wait for care that was life-saving,” Potter said. “That was absolutely not true. In [the U.S.], many people wait and never get the care they need because they’re either uninsured or underinsured.”
Like Tinani’s mother, many Americans have also delayed care amid the pandemic out of concern that they might spread or get exposed to the virus while sitting in a waiting room or standing in line for medications. Even routine childhood vaccinations nosedived during the pandemic, pushing the U.S. Department of Health and Human Services on Aug. 19 to allow pharmacists to train and qualify to administer vaccines to children ages 3 to 18, all in an effort to increase those rates and prevent mini-epidemics from spiraling amid COVID-19.
Quality and outcomes
When the U.S. health insurance industry smeared the Canadian system, they chose carefully selected points of attack, Potter said. They tossed into the echo chamber the fact that Americans stood a better chance of surviving breast cancer than Canadians. They neglected to say Canadians were more likely to live after a cervical cancer diagnosis than Americans. In fact, Canadians enjoy better health outcomes overall than Americans, from infant mortality to life expectancy. The COVID-19 pandemic belongs on that list, too.
Canada has about one-tenth of America’s population. During the COVID-19 pandemic, Canada has seen many fewer cases and illnesses, but the difference is not proportionate. More than 128,000 Canadians have gotten sick, more than 9,100 more have died, and cases have started to plateau, according to the latest data from Johns Hopkins University. But cases are accelerating in the U.S., which has become the global epicenter for the virus, with roughly 6 million confirmed cases and 183,000 deaths — or the equivalent of one in five COVID-19 fatalities worldwide.
One strength of the Canadian system to shine through during the pandemic is that everyone is insured, Martin said. There, patients admitted into hospitals don’t have to bicker over bills with insurance companies or double-check coverage before they rush to the hospital or ask for medical care. Hospitals work with a single insurer, she said, and that means care is better coordinated across institutions.
“Anybody that needs COVID care is going to get it,” she said.
Dr. Ashish Jha, who has directed the Harvard Global Health Institute and now serves as the dean of the Brown University School of Public Health, has a slightly different take. He said outcome disparities for coronavirus patients in the U.S. and Canada present “a reflection that has nothing to do with the underlying health system” but rather reflects leaders and their political will and priorities. While America’s health care system is among the world’s best in terms of innovation and technology, Jha said that U.S. political leaders have shown themselves to be unwilling to trade off short-term pain of lockdowns and job losses for a long-term public health crisis and economic instability. Those officials prematurely reopened the country before COVID-19 transmission subsided, he said. They also didn’t ramp up testing quickly enough to effectively monitor when and where outbreaks would occur and repeatedly undermined the public health community in its efforts to effectively respond to the virus. He said leaders in the U.S. have not offered a clear consistent message or decisive leadership to unite the country and get everyone moving in the same direction. During pandemics and times of national crisis, the public should not also worry about how to be smart consumers of health care, he said.
“It’s really frustrating to have to divert so much political energy towards what should be a no-brainer,” Jha said. “This is the time when everybody who needs to be tested, is tested — everybody who needs to be taken care of is taken care of.” And that starts with uniform access to effective health care, he said.
Why reform is hard in both countries
As the U.S. entered lockdown under coronavirus, Sen. Bernie Sanders announced on April 8 that he had pulled the plug on his presidential run. A week later he endorsed former Vice President Joe Biden. After contests in 28 states and two territories, his path to winning the Democratic nomination had narrowed significantly despite an early edge. The next month, in a gesture designed to appeal to Sanders’ heartbroken supporters, Biden announced plans to expand Medicare. His campaign has proposed offering “every American a new choice, a public health option like Medicare” to make insurance more affordable.
As Potter watches COVID-19 rage in the U.S., the former health care communications executive said Americans live in “fear of having big out-of-pocket bills without assurance that we’ll have our expenses covered.” With the number of uninsured Americans nearly double what they were before novel coronavirus, according to some estimates, Potter said that is not sustainable. In the latest PBS NewsHour-Marist poll, 56 percent of Americans think the U.S. response to the coronavirus pandemic was below average, if not the worst, in the world.
This pandemic could bring the country to a breaking point, Potter said, pushing more Americans to call for a health care system that goes beyond the reforms of the Affordable Care Act, which the Trump administration has repeatedly attacked and attempted to dismantle.
But if that happens, he said, the same private health insurance system that paid him to lie will reignite misinformation campaigns and fight hard to keep what it has.
“You will see this campaign resurface to try to scare people away from change,” he said. “It happens every time there is a significant push to change the health care system. The industry wants to protect the status quo.”
There’s no perfect health care system, and the Canadian system is not without flaws, Flood said. For years, debates have raged about expanding that nation’s health care system to include broader benefits covering few gaps where patients are still exposed to costs. In June 2019, New Democrat Party Leader Jagmeet Singh proposed expanding Canada’s pharmaceutical drug coverage. The eventual goal of these changes that have been debated in varying degrees for years is to encompass dental, vision, hearing, mental health and long-term care to create “a head to toe health care system.”
And yet it is natural for Canadians to compare systems with their neighbors and simply “feel grateful for what they have.” She says that kind of complacency has insulated Canada’s system from further improvements that produce generally better outcomes for lower costs, as in the United Kingdom, the Netherlands or Switzerland.
“As Canadians, we don’t push hard enough for the system to get better because we’re always relieved that at least it’s not the American system,” Flood said.
