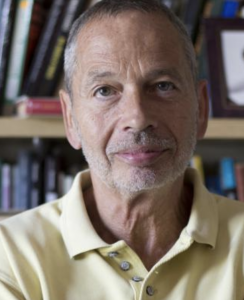
In 1997 Frank Furedi — an emeritus professor of sociology at the University of Kent — wrote a critically acclaimed book entitled, “How Fear Works: Culture of Fear in the 21st Century.”
In that book he tells the story of the public reaction to a magazine cover portraying a little girl fishing with her father. Some people, like Furedi, found the picture heartwarming. Others railed against the fact that, although the boat was in 2 feet of calm water, the girl was not wearing a life jacket.
He tells other stories: another father/daughter photo (this time cuddling) that the majority of viewers thought depicted a pedophile; and then the image of a child alone in a playground that evoked fears of kidnapping.
Granted, these are very selective anecdotes, used by Furedi to support his argument that we live in an age of anxiety — one of risk avoidance, alarmist reactions, and a prevailing narrative of threats we must be made aware of.
Extrapolating this to health care, although we may not always be proactive about improving our health, we certainly can be quite reactive when it comes to perceived threats to our health. Understanding these reactions requires understanding fear.
Our experience with fear
Journalists and PR people have figured out the clickbait value of fear. If you search our website with the keywords “fear” or “fear-mongering” you will get dozens of hits. This shouldn’t be surprising. After all, when it comes to our day-to-day health or lifespan, we see the stakes as high, near, and dear.
Take these recent examples of fear-mongering headlines we’ve spotted:
Sperm count drop ‘could make humans extinct’
Youth football changes nerve fibers in brain
Having just one energy drink can narrow blood vessels in 90 minutes, study finds
North Carolina man’s runny nose turns out to be leaking brain fluid
As ridiculous as these headlines may sound, they’re clearly attention-grabbing. One thing they all have in common is accentuating the most alarming aspect of a health concern, while minimizing or neglecting critical context.
For example, the sperm count story buries the fact that limitations of the research lead other experts to call the concern about human extinction “premature.” The football/ brain changes news release is a classic example of highlighting MRI results without making it clear that the clinical implications, if any, are unknown. The energy drink headline doesn’t explain that the study was designed to show how energy drinks affect the body — it can’t prove that just one drink leads to heart attacks or strokes. The runny nose story is an extremely rare anecdote, which makes the headline classic scare-mongering.
As we’ve mentioned before, headlines like these are usually misleading for one or more of the following reasons: They’re often based on observational studies, dramatic relative risks not absolute ones, rodent studies, very rare occurrences, or eye-catching surrogate findings that have little-to-no real world significance.
 And it’s not just news outlets that use scare tactics, but also academic medical centers, professional medical societies, health advocacy/awareness campaigns, and medical journals.
And it’s not just news outlets that use scare tactics, but also academic medical centers, professional medical societies, health advocacy/awareness campaigns, and medical journals.
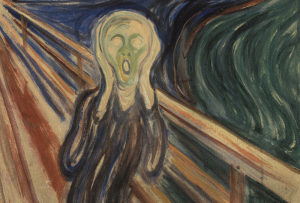
As we pointed out last week, studies suggest that novelty — especially when coupled with strong emotional responses like fear — holds strong allure.
At issue here is something quite critical: the interplay of risk communication and risk perception.
Risk communication and perception
A common scapegoat for poor risk communication is the media. But Furedi raises an interesting point in his book; that is, the media usually IS our major source of information, BUT mainly for things we don’t have direct experience with.
The implications of this for health care media messages — and risk communication in particular — is that most of us have very little “direct experience” until we become patients ourselves. Otherwise, our next closest thing to direct experience is via people we know, and our perception of risk is further complicated by many variables including age, gender, educational level, social class, and culture.
In other words, risk perception is highly individualized.
But risk communication is another story. It’s very much a media story.
Incomplete risk messages can lead to harm
When it comes to inadequate risk communication, media coverage of cancer screening is as good an example as any of how selectively playing up fear can lead to harm.
One need look no further than “Pinktober,” or Breast Cancer Awareness Month. The dominant message of this annual campaign is so consistent, coming from so many sources, that it’s almost become a tacit understanding … a foregone conclusion … in essence, a fossilized narrative: Get screened! Early detection could save your life!
This is pointed out to us by our newscasters, doctors, advocacy groups, billboards, sports teams, Facebook, celebrities, and even journalists.
As we wrote last October, what’s NOT pointed out is that, although there’s some truth to this narrative (some deaths from breast cancer can be averted through screening), there are other risks to be weighed:
“The Pink Message trumpets this relatively modest benefit and typically downplays or ignores potential harms and uncertainties, which are considerable. It’s estimated that between 20 and 50 percent of women over age 40, who are screened annually with a mammogram, experience at least one false alarm that leads to a breast biopsy. Others will be treated unnecessarily, possibly with surgery or toxic chemotherapy, for a cancer that never would have caused them harm.”
But we rarely hear this very important un-pink message: The injudicious use of breast cancer screening can lead to physical, financial, and emotional harms without cancer being diagnosed. The decision to get screened is a very personal one, and women should consider it carefully before taking any action.
How can any of us make an informed risk assessment without knowing all the risks? The prevailing narrative revolves around fear — fear of death from cancer to be exact — but isn’t based on evidence. It brings to mind this quote from Polish physicist/chemist Marie Curie:
“Nothing in life is to be feared, it is only to be understood. Now is the time to understand more, so that we may fear less.”
The sobering reality may be this: appealing to fear may be easier and more successful in terms of drawing attention than asking for the investment required by understanding.
And thoughtful risk communication should not be about fear, but understanding.