Even unvaccinated health workers had a lower rate of lab-confirmed cases than the overall community – 1.33 per 10,000 person-days versus 1.96, researchers concluded
Article content
There’s no doubt that health-care workers have been among the hardest hit by the pandemic.
Long, grueling hours, the stress of treating desperately ill patients and concern about catching the disease or passing it on to family members have made for a traumatic year.
But a just-released B.C. study has added to a surprising body of evidence about the pandemic. It suggested that people working in hospitals and other health-care facilities have actually been slightly less likely than others to contract the coronavirus.
The paper by researchers at the University of British Columbia and Vancouver Coastal Health – posted online but not yet peer-reviewed – seems to jibe with other studies, too.
That includes a federal report indicating that by last September rates of infection were about the same among health professionals and the general population.
Data do suggest nurses, personal-support workers and doctors seemed much more at risk of catching COVID in the first few months of the pandemic, especially in long-term-care facilities where infection-control procedures were lax.
Advertisement
Story continues below
This advertisement has not loaded yet, but your article continues below.
Article content
But that was at least partly a statistical anomaly, researchers theorize, the result of health-care workers having better access to testing in the first weeks of the crisis.
Article content
“We’re just not seeing a lot of transmission from infected people to health care workers when they use their equipment consistently and properly,” said Dr. Gerald Evans, head of the infectious disease division at Queen’s University medical school.
“There’s actually been very, very little in the way of transmission to health-care workers in the acute-hospital setting.”
Advertisement
Story continues below
This advertisement has not loaded yet, but your article continues below.
Article content
He pointed to a U.S. study that found it was also extremely rare for patients to catch COVID in a Boston hospital.
That’s a stark contrast to Ontario’s SARS outbreak in 2003, which was largely a “nosocomial” disease – spread within the health-care system – and took a heavy toll on nurses and doctors.
But the data from the B.C. study and others fail to convince some in the system, who believe nurses and others are still not being adequately protected from COVID-19 – and are suffering the consequences.
Article content
If there has been any improvement in safety for those workers over the last year, it’s because unions have pushed for better protection, said Linda Silas, president of the Canadian Federation of Nurses Unions.
“Doesn’t it make sense that health care workers that are dealing with patients with COVID-19 are getting sicker? They’re just closer to the action,” she said.
Advertisement
Story continues below
This advertisement has not loaded yet, but your article continues below.
Article content
“Close to 100,000 health-care workers were at some time out of the system because of COVID-19, and that is a very high number.”
There’s actually been very, very little in the way of transmission to health-care workers in the acute-hospital setting
Silas said raw data obtained from the Public Health Agency of Canada indicate that about 93,000 health workers had tested positive by late April, slightly above the seven per cent the agency says they represent in the Canadian population. But most case reports don’t include the patient’s occupation, so that number may be an under-estimate, she said.
Her view is certainly in line with the sense that formed early in the pandemic, as numerous doctors and nurses fell ill among northern Italy’s rampant outbreak and many staff at Canadian long-term care homes were infected.
“A lot of the information was actually based on the media reports of health-care worker impact,” said Dr. Lynora Saxinger, an infectious-disease specialist at the University of Alberta. “The public perception and indeed perception in healthcare workers is shaped by this kind of narrative. “
Advertisement
Story continues below
This advertisement has not loaded yet, but your article continues below.
Article content
To draw a more empirical picture, the British Columbia study looked at infection rates among health workers and everyone else in the greater Vancouver area from the beginning of the pandemic until May 13. Among health employees, doctors were least likely to contract COVID-19, while licensed practical nurses and care aides – many of whom work in long-term care homes – were most at risk.
With front-line health workers among the first to get vaccinated, their infection rate fell well below that of other Vancouver residents this spring, it found.
But even unvaccinated health workers had a lower rate of lab-confirmed cases than the overall community – 1.33 per 10,000 person-days versus 1.96, the researchers concluded.
Advertisement
Story continues below
This advertisement has not loaded yet, but your article continues below.
Article content

A Public Health Agency of Canada report in March said health-care workers – again, about seven per cent of the Canadian population – accounted for 20 per cent of COVID cases as of last September. But the rate peaked in May of 2020, and had steadily fallen to 6.5 per cent of new cases by the fall, said the analysis.
And the rate of severe illness and death was far lower among the health employees, the agency said.
Likewise, a Public Health Ontario study published in December found that infection among health workers – which had been as much as seven times the overall population earlier – was the same by September.
All the studies noted that limited testing at the dawn of the pandemic focused on the health-care sector, and could largely explain why that group produced more positives.
Advertisement
Story continues below
This advertisement has not loaded yet, but your article continues below.
Article content
There’s been a similar phenomenon in Alberta – more testing initially among health workers and eventually a similar or lower rate of infection, said Saxinger.
But how exactly is that possible? During the SARS outbreak in Ontario, 43 per cent of the 375 cases were nurses and doctors, with three of them dying.
The difference probably relates in part to the fact COVID patients tend to be most contagious early in the course of their infection, including before they actually develop symptoms, said Saxinger. Many don’t end up in hospital until days later, by which time they’re shedding less virus.
And then there is the better infection-control procedures imposed after SARS, she and colleagues say.
Yet those protective measures figure in one of the hottest debates around COVID-19.
Advertisement
Story continues below
This advertisement has not loaded yet, but your article continues below.
Article content
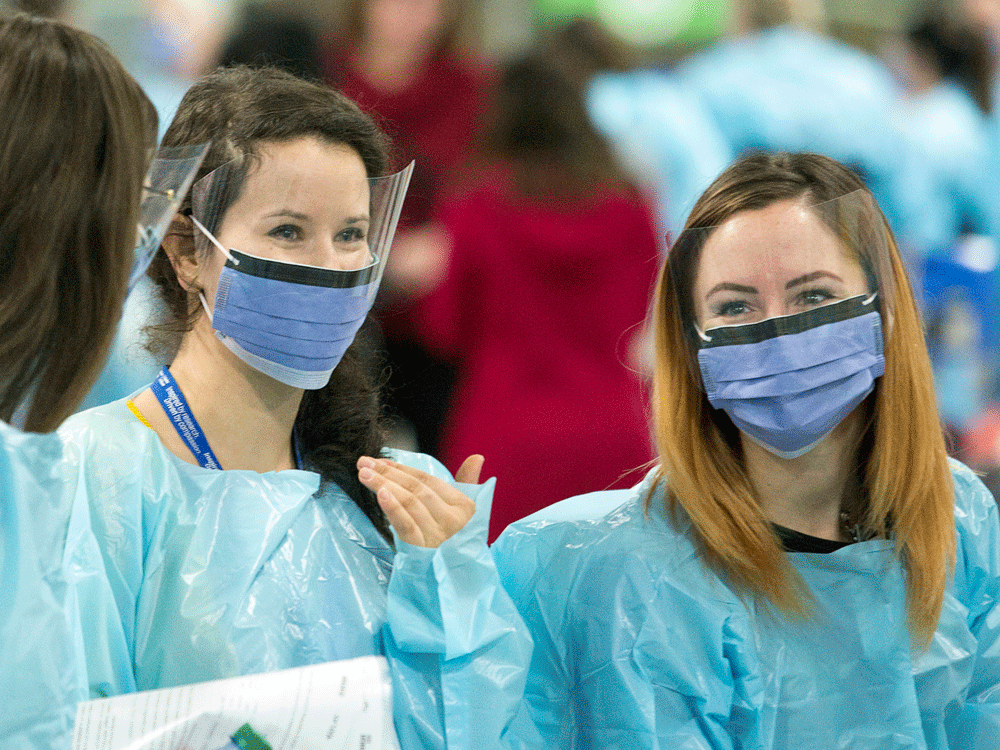
The current protocol in most of the country calls for wearing a surgical mask, gown and eye protection around known or suspected COVID patients, switching to a more impermeable N-95 respirator during “aerosol-generating” procedures and when judged necessary by staff members.
That approach has provided “excellent protection,” the B.C. study concludes, echoing the views of many infectious-disease physicians.
But Silas strongly disagreed, saying that nurses and others should be wearing N95 masks whenever they are within six feet of a patient. It shouldn’t be up to individual workers to request that kind of protection, she said.
• Email: tblackwell@postmedia.com | Twitter: tomblackwellNP
Advertisement
Story continues below
This advertisement has not loaded yet, but your article continues below.


