On this page:

Have you been diagnosed with early-stage Alzheimer’s disease, vascular dementia, Lewy body dementia, or a frontotemporal disorder and live alone? Or, do you have mild cognitive impairment (MCI)? If so, these tips are for you.
These tips offer ways to help you cope with changes in memory and thinking, prepare for the future, and stay active.
Use the table of contents at the top of this page to go to different sections. At the end of each section, click on the “Back to top” link to return to the table of contents.
Make Everyday Tasks Easier
Many people with early-stage dementia continue to manage their everyday activities. But it’s important to look ahead to a time when performing daily tasks will be harder. The sooner you adopt new strategies to help you cope with changes, the more time you will have to adjust to them. Here are some tips:
- Organizing your days. Write down to-do lists, appointments, and events in a notebook or calendar. Some people have an area, such as an entryway table or bench, where they store important items they need each day.
- Paying bills. Setting up automated payments is an easy way to pay your bills correctly and on time without having to write checks. Talk with your utility providers, insurance companies, and mortgage company or leasing office about automatic bill payment. Also consider asking someone you trust to help you pay bills. That person could review your financial statements and ask you about anything unusual.
- Shopping for meals. Many stores offer grocery delivery services. You can also order fresh or frozen meals online or by phone. Meals on Wheels America (1-888-998-6325) can deliver free or low-cost meals to your home, too, and this service sometimes includes a short visit and safety check. Other possible sources of meals include houses of worship and senior centers. If you make your own meals at home, consider easy-to-prepare items, such as foods that you can heat in the microwave.
- Taking medications. Several products can help you manage medications. You can try a weekly pillbox, a pillbox with reminders (like an alarm), or a medication dispenser. You can buy these items at a local drugstore or online. You may need someone to help you set these up. Or try an electronic reminder system, such as an alarm you set on your phone or computer.
- Getting around. If you drive, you may become confused, get lost, or need increasing help with directions. Talk with your doctor about these changes. Take seriously family and friends who express concerns about your driving. Some people decide to give up driving and learn how to use public transportation. For non-drivers, other forms of transportation may be available in your area, or you might want to consider a car or ride-sharing service.
For more suggestions on living independently, see Aging in Place: Growing Older at Home.
Scan Your Home for Safety
Making minor changes in your home can create a safer environment. For example:
- Get rid of unused items and extra furniture. If there are things you no longer use (such as clothing, appliances, decorations, and furniture) that are filling up your home, now is the time to remove them. Consider donating items in good condition to a charity. Some organizations will pick up from your home.
- Remove throw rugs. Move electrical cords and other things you might trip over. Falls can cause injury and disability and make living alone hard. For more fall prevention tips, such as using handrails, read Fall-Proofing Your Home.
- Install an automatic shut-off switch on the stove. If necessary, have your stove disabled. Instead, use a microwave or electric device with an automatic shut-off, such as a slow cooker or rice cooker, to heat up food.
- Set the water heater at 120 °F to avoid scalding tap water. Add nonskid mats to showers and tubs.
- Carry identification. Medical ID bracelets and necklaces are helpful in case you get lost or need help. Consider joining the MedicAlert + Alzheimer’s Association Safe Return program (1-800-432-5378). This is an emergency response system for people with Alzheimer’s disease or a related dementia.
- Consider safety devices. Other safety devices you may want to consider include fall monitors, emergency call buttons, and GPS tracking systems. Ask a relative or friend to help you buy the right device and set it up.
- Make sure smoke and carbon monoxide detectors are installed in or near the kitchen and all bedrooms. Check that the batteries are working. Set reminders to check the batteries every 6 months.
For more home safety tips, read the Home Safety Checklist for Alzheimer’s Disease.
Prepare for the Future

Preparing for the future may be the last thing you want to think about. But it will be easier to think about health and finances now rather than later to make sure you have a say in future decisions.
- Get legal and financial matters in order as soon as possible. Prepare or update your will, living will, healthcare power of attorney, and financial power of attorney. Call your lawyer or contact the National Academy of Elder Law Attorneys (1-703-942-5711) to find an attorney. Be sure to let someone you trust know where your documents are kept or give them a copy. Get more information and advice on legal and financial planning.
- Understand your options for in-home care. Family members and friends can often help with everyday activities. If you will need more help, look into options for a personal care assistant or home health care aide and their costs. For example, Medicaid recipients may qualify for a home health care aide, Medicare covers limited home services for people who cannot leave their homes, and the U.S. Department of Veterans Affairs may provide at-home care for some veterans. For more information on in-home care, read What Is Long-Term Care? and Paying for Care.
- Plan for what happens when you can no longer live alone. There will come a time when you will need more care and support. Could a family member or caregiver move in with you? Or could you move in with them? Professional home care, assisted living communities, and nursing homes are other options. Learn more about long-term care and how to pay for it.
- If you work, consider your options. You could share your diagnosis with your employer and discuss how to adjust your work. Under the Americans with Disabilities Act, employers with more than 15 employees are required to provide reasonable accommodations for people with disabilities. This might include changing your hours, getting reminders, or splitting up large tasks. Read Alzheimer’s and Employment from the BrightFocus Foundation for more information. If you are no longer able to work because of your condition, you may be eligible for disability income through private disability insurance (if you purchased this previously), Social Security, or veterans’ benefits. A Social Security program called Compassionate Allowances ensures quick review of disability claims for people with conditions including early-onset Alzheimer’s, Lewy body dementia, frontotemporal dementia, and some other types of dementia.
Strengthen Your Support System

Family members, friends, or other caregivers may be able to help in different ways. Here are some suggestions:
- Identify people you trust who can visit you regularly and be an emergency contact. Write down and save their phone numbers and other contact information in an obvious place, such as on your refrigerator door or in your wallet or mobile phone. If you have family members who live at a distance, they can still help. Read Getting Started with Long-Distance Caregiving.
- Visit a doctor or neurologist who can track changes in your memory, thinking, and ability to complete everyday tasks. Ask the doctor to provide a care plan and write down care directions (or have a family member or friend take notes during the visit). If travel is difficult, ask your doctor’s office about home visits or visits by phone or computer. The office also may help you find a home health care aide or geriatric care manager, a person who helps older people find services they need.
- Consider sharing your diagnosis with neighbors you trust. Neighbors are often the first people to notice if someone is wandering and looks lost and may be able to help or get help if needed.
- Learn about home- and community-based support and services. Social service agencies, local nonprofits, and Area Agencies on Aging can provide or refer you to in-home help, transportation, and meals to help you live at home. Call the Eldercare Locator (1-800-677-1116) to learn about services in your area, look on your State government or tribal organization’s website, or reach out to community centers and houses of worship. For more information on services, read Getting Help with Alzheimer’s Caregiving.
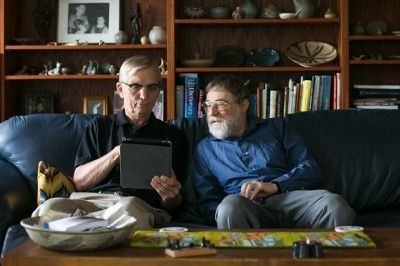
- Stay connected with technology. Smartphones, tablets, and smart speakers can help with things like the weather and time and connect you with family and friends through video chats, email, and social media. Some devices can help you find your keys and other important items. You may want to get products that are easy to use, such as a five-button remote control or a telephone with pictures for dialing. Whatever technology you consider, start early so you can learn the system and establish a routine. Are you unfamiliar with technology? Ask your local library or community center about classes.
- Talk with others who share your condition. The Alzheimer’s Association has a 24-hour helpline (1-800-272-3900) and both online and in-person support groups. Other support groups are also available online. Many NIA-supported Alzheimer’s Disease Research Centers offer programs to support and engage people with Alzheimer’s disease or a related dementia. Maybe your community has a memory café—a place to enjoy activities and socialize.
- Get help if you need it. If you feel down and are having suicidal thoughts, call the National Suicide Prevention Lifeline at 1-800-273-8255.
Keep Your Mind and Body Healthy

Being physically active, eating a healthy diet, getting enough sleep, and spending time with family and friends offer proven benefits. They may also help slow the symptoms of Alzheimer’s disease and related dementias.
- Exercise. You don’t have to join a gym or spend a lot of money. Even light housework, gardening, and walking around the neighborhood can have benefits. Experts recommend both aerobic exercise (such as walking) and strength training (such as lifting weights). Learn more about exercise and physical activity.
- Eat right. A healthy diet is proven to influence heart health, which relates to brain health. Learn more about healthy eating.
- Sleep well. Lack of sleep and poor-quality sleep are linked to memory problems. Try to get 7 to 8 hours per night.
- Be mindful. One way to help manage stress and reduce anxiety and depression is a technique called mindfulness. Mindfulness is being aware of what’s happening in the present, both inside and outside of your body. This web page and handout offer overviews of mindfulness in daily living.
- Stay social. People with dementia who live alone don’t manage daily activities as well when they feel lonely. Join a support group, chat with someone regularly, or volunteer at a local school or community organization. For example, you could read to children at the library. For more ideas, visit Participating in Activities You Enjoy.
This content is provided by the National Institute on Aging (NIA), part of the National Institutes of Health. NIA scientists and other experts review this content to ensure that it is accurate, authoritative, and up to date.
Content reviewed: November 12, 2019
